Recombinant insulin is human insulin made by genetically engineered microbes rather than by extracting the hormone from animal pancreases. It is produced by inserting the human insulin gene into bacteria or yeast and growing them in controlled tanks, where they manufacture insulin that is then purified. This process, a form of precision fermentation, has replaced animal-derived insulin in most of the world since the 1980s.
What is recombinant insulin?
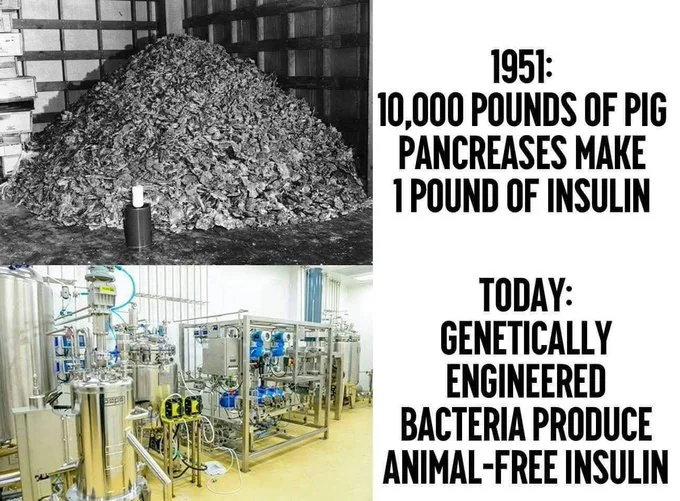
Recombinant insulin is bioidentical to the insulin naturally made by the human pancreas, but it is manufactured in microbial cell factories such as E. coli bacteria or yeast. It differs from older animal insulins (porcine or bovine), which required large volumes of animal tissue and could trigger immune reactions in some patients.
In 1982, the first recombinant DNA medicine, human insulin, was approved, marking the birth of modern biopharmaceuticals (NHGRI timeline).
Today, most insulin used clinically is either recombinant human insulin or engineered variants called insulin analogs.
How is recombinant insulin made?
Manufacturers follow a well-established bioprocess that does not involve animals:
- Design the gene: The DNA sequence for human insulin (or a modified analog) is prepared and inserted into a plasmid, a small circular DNA molecule.
- Engineer the microbe: The plasmid is introduced into a production strain of E. coli or yeast (for example, Saccharomyces cerevisiae or Komagataella phaffii), turning the microbe into a “cell factory.”
- Precision fermentation: The engineered microbes grow in sterile bioreactors fed with sugar, nutrients, and oxygen, expressing insulin or a precursor (proinsulin) in large amounts.
- Downstream processing: Cells are harvested and broken open, insulin is captured, enzymatically processed to the final two-chain form if needed, folded, and extensively purified.
- Formulation and fill-finish: The purified protein is formulated with stabilizers, sterile-filtered, filled into vials or pens, and quality tested.
Detailed production strategies and host systems are reviewed in Baeshen et al., Microbial Cell Factories. Although genetically modified microbes are used during manufacturing, purification and extraction ensure they are not present in the final medicine, a point consistent with food-grade precision fermentation processes (precision fermentation overview).
Purification and extraction steps ensure genetically engineered microorganisms are not present in final products, even when they are used during production (precision fermentation).
Why did recombinant insulin replace animal insulin?
- Purity and consistency: Recombinant production achieves very high purity and batch-to-batch consistency compared with pancreas extraction.
- Lower immunogenicity: Human-sequence insulin reduces allergic reactions that some patients experienced with bovine or porcine insulin.
- Scalability: Bioreactors can produce large, reliable volumes without relying on slaughterhouse byproducts.
- Supply ethics and resilience: No animals are used, and supply chains are more controllable.
These advantages drove a global transition to recombinant products soon after their approval in the early 1980s.
Are insulin analogs different from recombinant human insulin?
Insulin analogs are also made recombinantly but include small amino acid changes that alter how fast they act or how long they last. Examples include rapid-acting analogs such as lispro and aspart, and long-acting analogs such as glargine and degludec. These modifications help patients better match insulin action to meals and basal needs. Clinical guidance on types and uses is available from the American Diabetes Association (ADA: Insulin basics).
Is recombinant insulin safe?
Yes. Recombinant human insulin has been used for more than 40 years and is regulated as a biologic medicine. Manufacturing is performed under strict Good Manufacturing Practices, with extensive controls on identity, purity, potency, and sterility. The production organisms and their DNA are removed during downstream processing, so the final drug contains only purified insulin. Broader safety and regulatory context for precision fermentation is summarized in a 2024 FAO report (FAO, 2024).
Why is insulin expensive in the United States?
High U.S. list prices reflect factors beyond manufacturing cost, including a concentrated market for brand-name analogs, complex patent portfolios around formulations and devices, and rebate and pharmacy benefit manager dynamics that incentivize higher list prices. Independent analyses detail these drivers and recent policy changes such as Medicare’s $35 monthly cap for many beneficiaries (KFF overview). Over 2023–2024, major manufacturers announced list-price reductions and expanded patient affordability programs, but out-of-pocket costs still vary by insurance coverage.
Manufacturing insulin via precision fermentation is efficient, yet U.S. patient costs are driven by pricing, rebates, and coverage design rather than production expense (KFF).
What does this mean for biomanufacturing more broadly?
Recombinant insulin demonstrated that precision fermentation can deliver essential, animal-free proteins at pharmaceutical scale. The same tools now produce food enzymes and dairy proteins without animals, illustrating the technology’s versatility (precision fermentation; Perfect Day process).